Introduction: The role of functional imaging in Multiple Myeloma (MM) has evolved in recent years due to the increasing availability of high platform imaging and the prognostic information of imaging response after treatment, as observed in PET/CT studies. Diffusion weighted whole body MRI (DW-MRI) is a functional imaging technique with an emerging role in the management of MM patients (pts) due to its high sensitivity, but consistent data regarding its prognostic role in the detection of residual disease after treatment in MM are lacking. The Myeloma Response Assessment and Diagnosis System (MY-RADS) imaging recommendations have been recently published (Messiou C et al, Radiology 2019) in order to promote standardization in response assessment. Criteria for Response Assessment Category (RAC) have been proposed with a 5 point scale defining the probability of complete imaging response (i.e. RAC 1) or progressive disease after treatment (i.e. RAC 5), but this score still needs to be validated in clinical practice. For this purpose, we performed an external validation of RAC criteria according to MY-RADS in newly diagnosed MM pts in order to evaluate the prognostic role of this technique after autologous stem cell transplantation (ASCT). Furthermore, we tried to correlate the results of MY-RADS with those of minimal residual disease (MRD) assessment by flow cytometry (FCM).
Patients and methods: We retrospectively analyzed the outcome of 60 MM pts (median age 63 years) diagnosed between January 2016 to January 2020 who underwent DW-MRI evaluation to assess the response at day +100 after ASCT, before maintenance. After anonymization, images were reviewed according to MY-RADS by Radiologists who were blinded to the results of clinical and biological data. Post ASCT Progression free survival (PFS) was calculated from the date of last ASCT (the second one in case of double ASCT) until progression or death from any cause. The predictive role of MRI RAC response on outcome was analyzed. Bone marrow samples were collected before maintenance for MRD by 8-color FCM (sensitivity 10-5). In pts with MRD evaluations, exploratory PFS analysis was performed; concordance between MRD and DW-MRI results was calculated and the level of agreement was expressed by Cohen's kappa statistics.
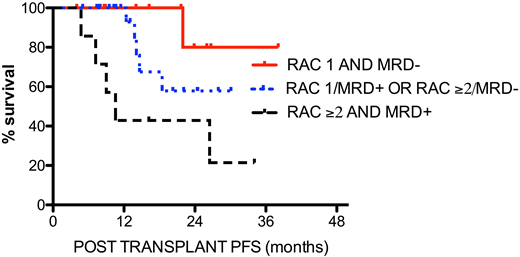
Results: out of 60 pts, 21 (35%) were ISS stage 3 and 13 (22%) showed high risk cytogenetics. Pts were treated with the following induction regimens: VTD 51, VRD 4, Dara-VRD 3, VCD 1, KRD 1. Single ASCT with MEL200 conditioning was performed in 41 pts (68%), %), whereas 19 patients (32%) received double ASCT. Response rates were VGPR 18,3%, CR 51,6% and sCR 13,3%. MRD before maintenance was available for 44 pts and was positive in 20 (45,5%). According to MY-RADS, a complete imaging response after transplant was observed in 36 (RAC 1: 60%). Some residual MM was identified in 24 (40%) [RAC2: 20 (33%), RAC3: 3 (5%), RAC4: 1 (2%), respectively]. After a median of 28 months, post ASCT PFS was significantly longer in pts with RAC 1 vs RAC ≥2: median NR vs 26,5 months, p 0,017, HR 0,29 (95% CI: 0,10-0,80). Concordance between WB-MRI and MRD results was low (52%, kappa 0,017: 16% both positive, 36% both negative). PFS according to DW-MRI response and MRD was significantly better for pts DW-MRI RAC1 and MRD negative before maintenance, compared to pts with RAC ≥2 and MRD positive results (PFS NR vs 10,6monts; p 0.012, HR 0,11 - 95%CI: 0,02-0,62). Intermediate PFS was observed for pts with either imaging or MRD positive results (PFS NR), with a significantly different outcome of the three subgroups (p 0,021) Figure 1. In 30 pts achieving CR or sCR, residual disease was identified in 14 (47%); in 4 of them by FCM only, in 8 by DW-MRI only, including two pts in sCR, and in two by both techniques.
Conclusion: given the high rates of CR seen in pts with MM with new treatment approaches, DW-MRI is a powerful tool to better evaluate the prognosis of pts treated with novel combinations and ASCT. Our external validation of RAC criteria highlights the ability of DW-MRI to stratify pts with different outcome and promotes the standardization in reporting functional imaging response after treatment. The low concordance between DW-MRI response and MRD results suggests that these two techniques may be complementary for the definition of response: their combined use could help clinicians to better refine the prognosis of MM pts achieving CR
Belotti:Amgen: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Jannsen: Membership on an entity's Board of Directors or advisory committees. Rossi:Jazz: Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees; Sanofi: Honoraria; Novartis: Other: Advisory board; Astellas: Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees; Daiichi Sankyo: Consultancy, Honoraria; Pfizer: Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria; Celgene: Membership on an entity's Board of Directors or advisory committees; Alexion: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal